Blue Cross and Blue Shield latest insurer to suspend deductibles or copays for coronavirus-related medical services
Blue Cross and Blue Shield announced Thursday that its network of locally-operated BCBS plans across the country will be waiving cost-sharing for the treatment of COVID-19 through May 31. This includes coverage for examinations and coronavirus treatment, including inpatient hospital stays.
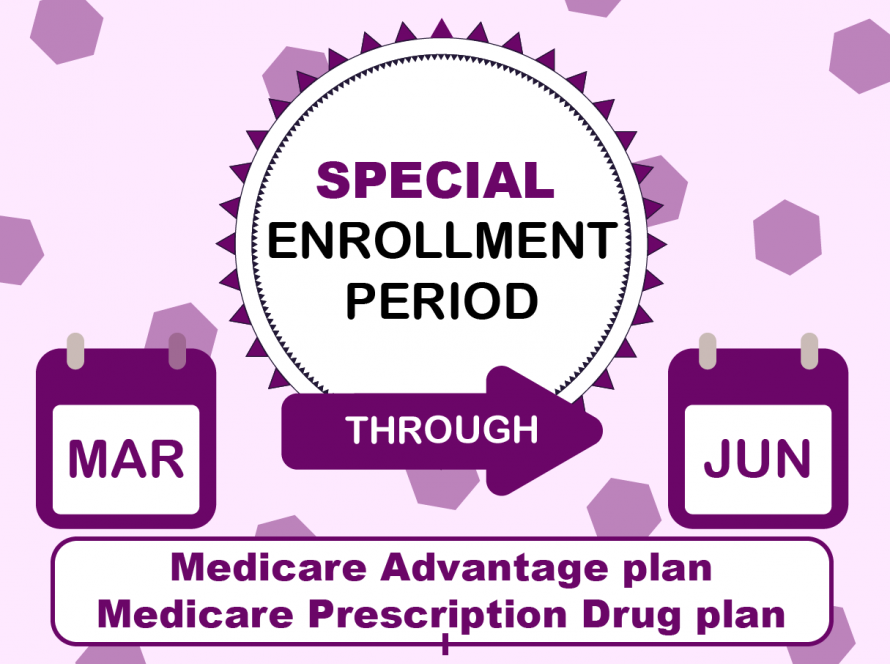
The plan is a part of a growing number of insurers that are cutting out-of-pocket costs for their members. This situation generally applies to most commercial plans and individuals with Medicare Advantage plans, Medicare supplemental or Medigap policies, and Medicaid.
In a Rose Garden briefing last Sunday, President Trump announced that two insurers, Humana and Cigna, would be waiving treatment-related charges such as copays and deductibles. These two national insurers join seven other large and small insurers who have taken such actions in the recent days.
Here are the announcements from other major insurers.
Aetna is waiving cost-sharing for inpatient admissions at all in-network facilities for treatment of COVID-19 or health complications associated with the pandemic. This policy applies to all Aetna-insured commercial plans and is effective through June 1, 2020.
AllWays Health Partners is removing copays, deductibles, or coinsurance for testing and copays for treatment for all in-network facilities; safeguarding access to out-of-network providers for the initial COVID-19 test or treatment when no in-network providers are accessible; and removing all cost-sharing for telemedicine services, including virtual distancing visits with primary care providers and specialists.
CareFirst is waiving copays, coinsurance and deductibles for in-network or out-of-network visits to a provider’s office, as well as for telehealth, lab fees or treatments related to COVID-19 “for the duration of this public health emergency.” It is also eliminating prior authorization requirements for medically mandatory diagnostic tests and covered services related to COVID-19 diagnosis.
Fallon Health is waiving copays for coronavirus treatment as well as loosening the rules for administrative procedures, such as prior authorizations and out-of-network requirements, for medically mandatory emergencies.
L.A. Care in California is waiving all costs associated with screening, testing and medically necessary treatment for COVID-19.
For more information: Click Here
References:
Bunis, Dena, AARP 2020, accessed 12 January 2021, < https://www.aarp.org/health/health-insurance/info-2020/coronavirus-insurers-treatment-costs.html >